
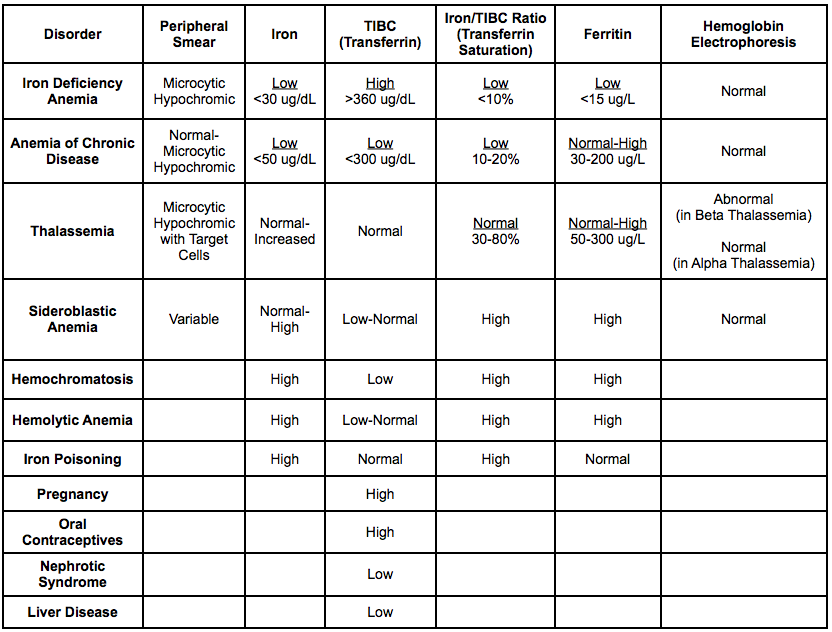


Infants and toddlers (refer to Iron Deficiency and IDA in Infants, Children and Adolescents).3 Use a case-finding approach to identify patients at risk of iron deficiency and iron deficiency anemia ( Table 1). Screening of the general population for iron deficiency is not recommended. TOP Identification of Patients at Risk for Iron Deficiency and Iron Deficiency Anemia IDA may be normocytic if anemia is mild or in early iron deficiency. The following laboratory findings are typical for IDA: microcytic anemia, hypochromia, and decreased ferritin. Iron deficiency anemia (IDA): anemia due to insufficient body iron stores 1. 1A hemoglobin value below the local, lab-specific lower reference interval indicates anemia. Iron deficiency: insufficient total body iron stores, caused by increased requirements, decreased intake, increased loss, and/or decreased absorption 1 (see Table 1).Īnemia: low hemoglobin level, most frequently defined as a hemoglobin value over two standard deviations below the gender- and age-adjusted mean. Consider prescribing IV iron when there is inadequate response to oral iron, intolerance to oral iron therapy, or ongoing blood loss.Continue oral iron for 4–6 months after anemia corrects to replenish iron stores. One preparation is not preferred over another patient tolerance should be the guide. Prescribe oral iron supplements as first line therapy for iron deficiency.Caregivers of infants and toddlers should receive guidance to prevent excessive cow’s milk intake.Take a nutrition history and provide dietary education to address dietary risk factors.Serum iron, iron binding capacity, and transferrin saturation/fraction saturation are not routinely useful for investigating iron deficiency anemia.The suggested cut-offs are estimated ranges that should be interpreted using clinical judgment based on the patient’s age, gender, risk profile ( Table 1) and symptoms. Ferritin is the test of choice for the diagnosis of iron deficiency.Iron deficiency by itself causes symptoms for patients, even in the absence of anemia, and warrants investigation and treatment.Consider age and clinical presentation when investigating for cause. Determine the cause of iron deficiency.There is no indication for population-based general screening. Use a case-finding approach to identify individuals at risk of iron deficiency and iron deficiency anemia ( Table 1).This guideline provides recommendations for the diagnosis, investigation and management of iron deficiency in patients of all ages. Iron supplementation for non-anemic pregnant women.Iron Deficiency and IDA in Infants, Children and Adolescents.Investigation of overt and occult GI and GU bleeding.Investigation of the Etiology of Iron Deficiency.Additional tests for the diagnosis of iron deficiency in patients with chronic disease, inflammation or malignancy.Identification of Patients at Risk for Iron Deficiency and Iron Deficiency Anemia.The TIBC is therefore a surrogate for a transferrin level and these two laboratory tests can be used interchangeably (usually the lab will only report one or the other).Effective Date: ApRecommendations and Topics.UIBC is the amount of "free" transferrin, unassociated with iron.Total iron-binding capacity (TIBC) and unsaturated iron-binding capacity (UIBC) Interpretation of Abnormal Iron Studies ConditionĤ5%) transferrin saturation suggests there may be an iron overload state such as haemochromatosis (or, that a patient has recently had an iron infusion). In brief, this complex topic can be reduced to a table.
#Iron studies interpretation free#
The best published resources for this topic would have to be this article by Hawkins et al (2014) and a free online guide to laboratory diagnosis of iron deficiency published by Dr Gross at The candidate with infinite time resource may be interested in this reporting standards statement from the Australian Royal College of Pathologists. Question 9.2 from the first paper of 2017 (acute phase response).Question 22.1 from the second paper of 2016 (a massively elevated serum ferritin level).The identical Question 18.1 and Question 18.2 from the first paper of 2015.Question 12.1 and Question 12.2 from the first paper of 2019.Question 24.1 from the first paper of 2020 (HLH).Question 18 from the second paper of 2021 (HLH).This topic has appeared with increasing frequency in recent exam papers:


 0 kommentar(er)
0 kommentar(er)
